The World Health Organization is clear about it: diabetes has turned into a global pandemic, with over 420 million people worldwide suffering from type 1 or type 2 diabetes. To get a clearer view of the magnitude of this health problem, we can try to condense data and imagine that the whole population of the U.S. (i.e. 332,915,073 inhabitants) plus Mexico (i.e. 130,262,216 inhabitants) suffer from diabetes. According to The American Journal of Managed Care, in the U.S. alone, a new patient is diagnosed with diabetes every 17 seconds! Diabetes is a pressing global health problem. That’s a proven fact. But are health organizations ready to address it? Can technology help? In today’s article, we will try to take a closer look at the way health organizations address this problem, see to what extent technology can help, and – ultimately – raise awareness about this silent enemy with devastating effects.
A wake-up call!
Back in February 2020, the International Diabetes Federation updated figures on diabetes on a global scale. The predictions are devastating: by 2045, 700 million people will be suffering from diabetes. Below you can check the most relevant data:
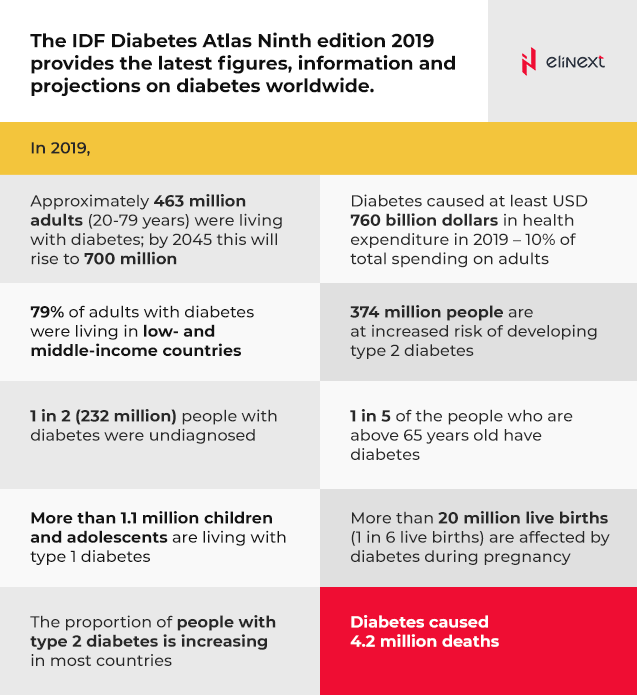
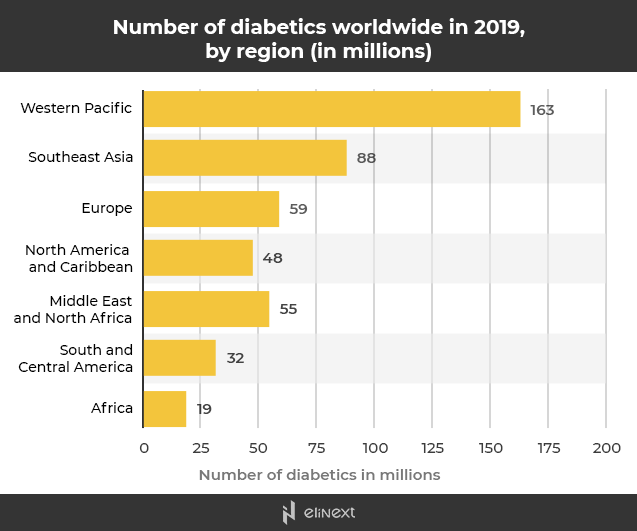
According to Statista, the Western Pacific region has the highest number of diabetics in the world, with approx. 163 million persons suffering from this condition. However, data in Southeast Asia and Europe is not precisely gratifying either. Even if the number of people suffering from diabetes in Africa seems to be low, we will see that the number of diabetes-related deaths in this region contradicts the apparently positive figures.
This Statista report clearly shows that Africa ranks third when it comes to premature diabetes-related deaths. Africa is only surpassed by South East Asia and Western Pacific.
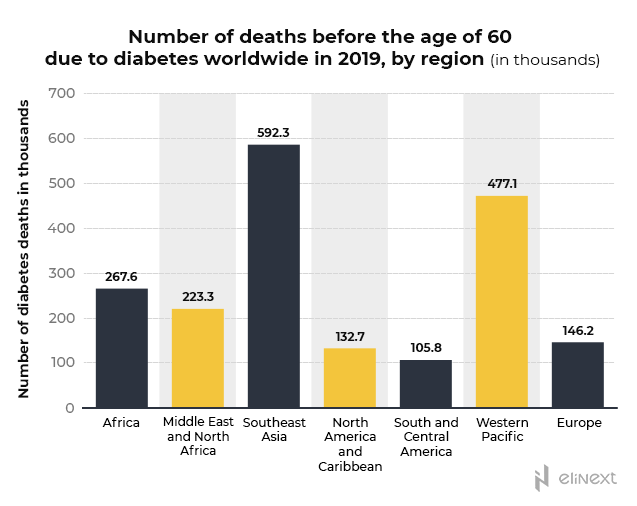
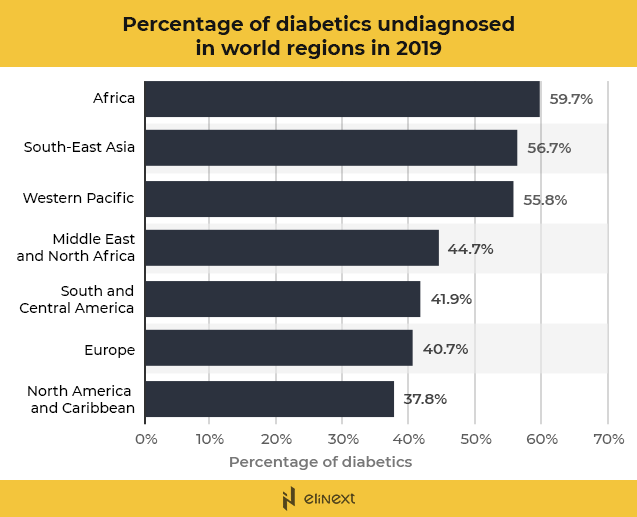
And there is a good reason for Africa to rank so low in the stats regarding the number of diabetics and so high in the stats that display the diabetes-related number of deaths. This Statista report shows that, in Africa, almost 60% of the adults suffering from diabetes are undiagnosed. No diagnosis = No treatment = No control = Premature death. A blunt equation with dreadful consequences.
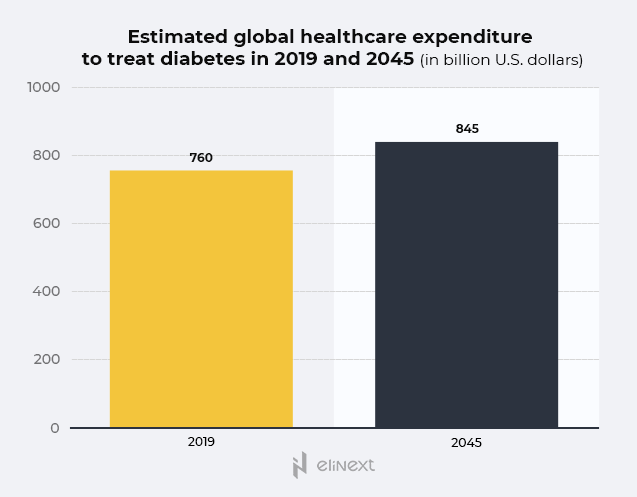
Another Statista report shows that, from 2019 to 2045, the expenditure for diabetes treatment at a global range is expected to reach an impressive 845 billion U.S. dollars, with China and the U.S. registering the highest diabetes-related medical expenditures. Despite their leading position when it comes to general diabetes-related medical expenditures, they do not hold the record for the highest spending per patient. The country that spent the most per diabetic patient in 2019 is Switzerland.
Even if figures and stats should raise concerns by themselves, we are talking about dry, aloof data. Understanding exactly how and to what extent diabetes undermines people’s health and lives might help people assemble the final picture and raise awareness.
Why is diabetes a global problem?
Back in 2019, the World Health Organization ranked diabetes 9th on the list of 10 leading causes of deaths. From 2000 to 2019, an impressive 70% increase was registered.

Unlike cancer, pulmonary diseases, or heart conditions, diabetes is not only a silent and underestimated enemy that often goes under the radar during regular medical check-ups but it is also a widely underreported disease as a cause of death. A late diagnosis and deficient disease management (by both patients and professionals) can lead to serious complications that put a severe strain on the already overworked health systems around the globe. Given the previously seen data that clearly demonstrates that the prevalence of diabetes is steadily rising, there is no wonder that many experts (e.g. Zimmet, P.Z.) consider diabetes to be the largest epidemic in the history of humankind. Leaving aside genetic susceptibility, physical inactivity, poor eating and sleeping habits, obesity, aging, and – ultimately – modernization are some of the factors that contribute to developing diabetes.
Health Complications
Diabetes is closely related to potentially deadly health complications such as cardiovascular diseases, nerve damage, hypertension (a condition that raises the risk for heart attacks and strokes), kidney disease, eye damage, skin conditions, higher risk of infections, or amputations. In fact, most people with diabetes die from cardiovascular complications such as heart attacks or strokes.
Quality of Life
Since diabetes is a chronic disease, living with it is not only stressful but also demanding. Diabetic patients not only constantly worry about the possible health complications they may develop but they also have to deal with the on-spot unpleasant symptoms caused by high or low blood sugar levels: anxiety (and even panic attacks), dizziness, irritability, tiredness, excessive hunger and thirst, nausea, blurring vision, shakiness, irregular heartbeat, or sweating. Dealing with diabetes is an always-demanding reality that forces diabetic persons to carefully plan and control each meal, exercise regularly, constantly monitor blood glucose levels, have regular blood tests, or follow the treatment plan. Given the lifelong psychological and physical burden imposed by this condition, people diagnosed with diabetes frequently have to deal with depression as well.
Why is it important to constantly monitor blood glucose levels?
Keeping blood sugar levels in the target range not only helps to delay and prevent long-term health complications but also improves the quality of life. Currently, people suffering from diabetes can monitor their blood glucose levels using either a self-testing blood sugar meter or a CGM (i.e. continuous glucose monitor) that consists of a small sensor that is inserted under the skin and provides continuous glucose information. There are several reasons why monitoring the blood glucose level is a crucial factor in dealing with diabetes:
- Measure and track the efficiency of the treatment
- Helps patients see if the diet and exercise routines have the expected results
- Helps patients understand how blood sugar levels change under specific circumstances (e.g. stress, infections, colds, etc.)
- Identify low and high blood sugar levels
Tendencies in the digital diabetes care market
As foreseen by MarketsAndMarkets, by 2024, the digital diabetes management market will reach $19.98 billion, at a CAGR of 23.8% if compared to 2019.
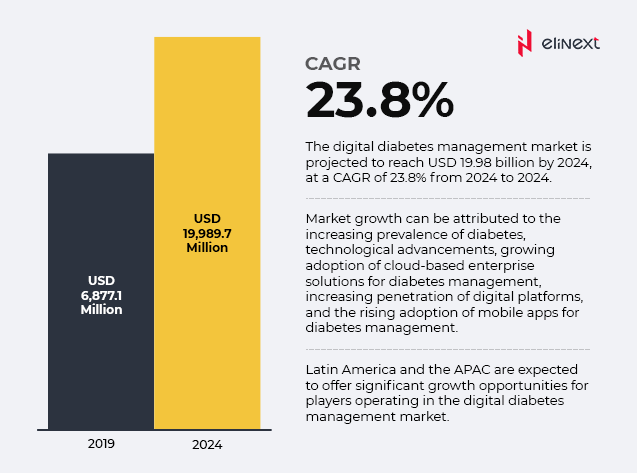
The prevalence of diabetes around the globe is continuously rising, giving birth to a pressing demand for improved and flexible solutions for diabetes care. Thanks to the impressive technological advancements, diabetes patients and professionals can now benefit from digital diabetes management solutions such as diabetes apps, data management software and platforms, or smart devices (e.g. CGMs, smart insulin pens and pumps, insulin patches, etc.) According to the same source, by 2024, the devices segment for digital diabetes management will be dominated by smart devices and apps. This growth has been fuelled by the general growing demand for wearable and wireless devices and the increased usage of connected apps and devices to ease virtually any facet of our lives.
However, digital diabetes management is not the land of milk and honey. While it is true that digital diabetes solutions are still in their nascent days and many challenges are yet to be overcome, the expectations are huge. Let’s take a look at the main advantages and disadvantages digital diabetes solutions provide to the end-user.
Advantages
- Seamless data
Digital tools are able to capture data seamlessly, offering patients and physicians valuable insights on the efficiency of the adopted treatment, thus supplementing and improving the medical practice
- Usage comfort
Traditional glucose meters imply pricking the skin using a lancet. Since diabetic patients need to control their blood glucose levels several times a day, this process is not only painful and uncomfortable but can also lead to skin infections. When it comes to usage comfort, CGMs or insulin pumps are like a breath of fresh air.
- Enhanced safety
For instance, automated bolus calculators have been reported to prevent insulin dose stacking and reduce hypoglycaemia. CGM devices allow patients to incorporate alarms to alert them of rapid glucose drops or rises.
- Self-education value
Since patients are able to constantly monitor their blood glucose levels, they can make valuable correlations between the registered values and their daily habits, thus being able to make corrections and adjustments
Disadvantages
- High cost
If compared with the traditional blood glucose meters, the price of performant insulin delivery devices (e.g. CGMs or smart insulin pumps) is significantly higher. If we add the costs of the associated consumables to the equation (e.g. insulin, patches, etc.), it becomes obvious that smart devices are practically out of reach for many end-users, a situation aggravated by deficient reimbursement policies. In fact, in many countries (e.g. China or India), diabetic patients need to fully bear the expenses for blood glucose monitoring, while in others (e.g. Spain) only insulin-dependent patients are eligible for reimbursements. The adoption of smart solutions in under-developed countries that barely have access to essential health services is completely out of question.
- Digital literacy
It’s no novelty for anyone that the younger population is more proficient at using new technologies than the older population. As a consequence, digitally illiterate patients can find themselves excluded.
- Overwhelming amount of data
Sometimes, having access to too much data can turn into an extra burden. That happens especially when patients see values outside the targeted range and lack the necessary training to interpret them correctly. Often, this triggers anxiety and even panic attacks.
Game-changing mHealth tools for diabetes management
While it is true that digital diabetes management tools are not widely used yet, we are talking about a game-changing innovation field meant to improve prevention, self-management, and self-education. mHealth solutions make use of SMS (text messaging), wearables, or smartphone apps to help diabetic patients improve self-care. Let’s see some relevant examples.
Continuous Glucose Monitors (CGM)
CGMs are compact medical systems designed to continuously monitor blood glucose levels in real-time (approx. every 5 minutes). CGMs consist of a small sensor and a small plastic tube that patients insert under the top layer of their skin (generally on the abdomen or arm). The sensor is held in place via a waterproof adhesive patch. What CGMs basically do is read glucose levels in the interstitial fluid and, with the help of a small transmitter, sends the registered values to the monitor device or to the smartphone app. Additionally, diabetic patients can opt to receive alarms when blood glucose levels are too low or too high. Among the CGMs that are currently available, we can highlight Dexcom G6 CGM (compatible with Dexcom’s Clarity mobile app and software), Medtronic’s Guardian Connect, or Abbott Diabetes Care’s FreeStyle Libre.
Insulin pumps for easier and safer insulin management
Insulin pumps are small electronic gadgets that the patient needs to attach to his/her body and generally consist of an insulin reservoir, the pumping mechanism, control buttons/touch screen, tubing, and an infusion set. Insulin pumps have been thought out to mimic the normal functioning of the pancreas and deliver the necessary dosage of short-acting insulin or specific insulin doses depending on the bolus. Thanks to technological advancements, insulin pumps are now compounded with CGMs, thus creating ‘closed loop’ systems (i.e. an artificial pancreas) that automatically monitor blood glucose levels and dose insulin. Tandem Diabetes Care’s X2, Medtronic’s Minimed 670G or 770G, Omnipod’s DASH system, or Valeritas V-Go are some of the available models.
Diabetes Management Apps
From mobile blood glucose trackers to calories counters, exercise logs, or all-inclusive apps, diabetic patients can access a wide variety of apps specifically thought out to reduce the burden of living with diabetes. For instance, Glucose Buddy is a free app (with available premium features) that allows users to track meals, blood glucose levels, medication, or physical activity. This app puts at the user’s disposal a rich food database and offers nutrition information on products by simply scanning the bar codes. It also includes a special diabetes education plan. The available options include apps such as Diabetes Tracker (MyNetDiary), Noom, or mySugr.
What solutions are still missing?
Undoubtedly, digital diabetes management solutions can provide patients with all the necessary means and data to significantly improve self-care. And that includes extra safety, extensive support, and – most importantly – comfort and peace of mind. However, there is a lot of room for improvement. Here are some aspects that require further attention not only on the part of the developers but also on the part governments and global health organizations.
Improved accessibility
We have already mentioned that older people are reluctant to using digital devices. And that mainly happens due to a lack of digital literacy. To address this problem and raise acceptance among our seniors, apps and smart devices developers should take into account the level of technological proficiency of the target user. Additionally, physical or mental disabilities (e.g. blindness or dyslexia) should also be kept present.
Geographical and economic barriers
Diabetic patients who live in isolated regions without Internet or who economically struggle for survival can hardly benefit from digital devices. Additionally, most apps are not free to download and use. The only solution to overcome these barriers is by means of special programmes to subsidise – at least partially if not totally – the use of smart devices by socioeconomically deprived diabetic patients.
Enhanced data security
We live in a digital world in which data security has become a main concern for all the obvious reasons. Usually, diabetes devices and apps allow patients to monitor their data and share it with their physicians. However, the concern is there, demanding enhanced cybersecurity solutions.
Improved performance
In order for a digital diabetes management tool to be useful and safe to use, it needs to be accurate and reliable. Even though the accuracy and clinical validity of certain digital diabetes management solutions have made the object of a whole series of studies, further research is still necessary.
Keep up with technological advancements
Technology advances at a rapid pace. And diabetes digital management devices make no exception, as it is of vital importance for these tools to keep up with the latest advancements (e.g. operating systems, platforms, connectivity, new features, etc.) Sometimes, patients and physicians alike find it difficult to assimilate novelty. Under an ideal scenario, physicians should be able to offer proper guidance to their patients. That can only be achieved if health care professionals undergo continuous and extensive training.
Wrap up…
While it is true that the sinuous path towards utmost accuracy, safety, reliability, and affordability has just begun and many barriers are yet to be overcome, new technologies have the power to improve the diabetes management process and, as such, ease the psychological and physical burden of many diabetic patients.