For over two years now, the world has been fighting COVID-19 with varied success. The toll that the pandemic has already taken on humankind is huge — millions of deaths, nationwide lockdowns, and upended economies. And now we are heading into the 7th wave of the pandemic, driven by the newest Omicron BA.5 subvariant.
And although coronavirus is on top of everyone’s mind, this virus is not an outlier but rather a part of the pattern typical for our connected world. Urbanization, climate change, and an increasingly mobile global population are powering the rising rate of outbreaks. According to WHO, there are 7,000 signals of potential outbreaks every month.
To top it off, each year hospital-acquired infections (HAI) impact almost 2 million patients and result in the death of 100,000 of them, which makes it yet another pressing challenge that healthcare organizations have to face.
Technology is stepping up to help humanity and healthcare systems address these problems more efficiently and at a global scale. From advanced thermal cameras that detect elevated temperatures to intelligent crowd monitoring and face mask detection systems, healthtech startups and tech giants are redefining the healthcare industry through innovative healthcare solutions. However, special attention is on building robust infection control and prevention systems that would help take outbreaks under control.
Benefits of infection control software
A well-designed infection control solution can go a long way towards helping healthcare institutions adapt to the ever-changing environment and optimize their prevention strategies.
Advantages for healthcare organizations:
- Streamlined workflows and reduced burden on healthcare staff
- Decreased costs without diminishing the patient experience
- Cross-departmental coordination
- Real-time access to actionable insights
Benefits for patients:
- Faster infection treatment and better health outcomes
- Shorter hospital stays
- Appropriate courses of antibiotics
What are the components of an infection control solution?
Although the features and components can vary depending on the needs of a particular healthcare institution, here are the basic and most important modules to consider:
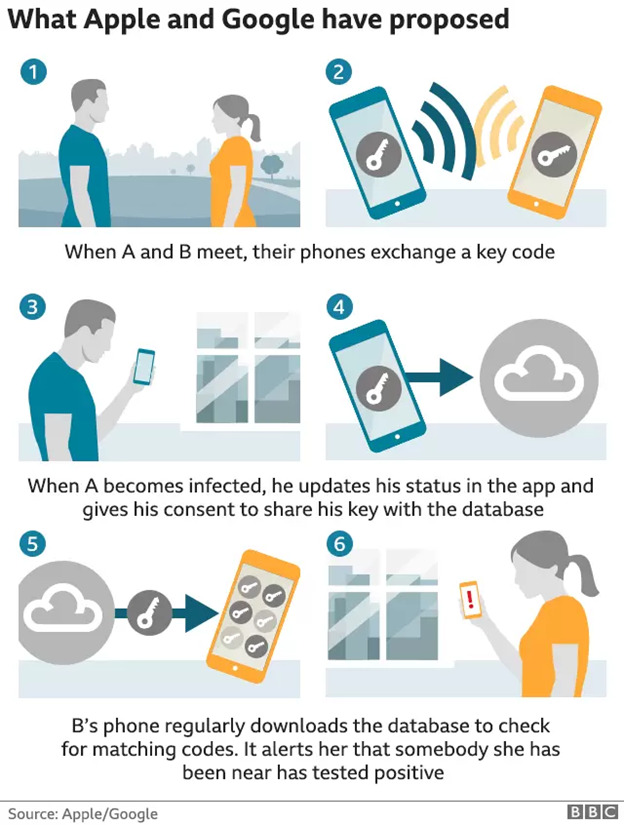
Contact tracing
Contact tracing is a monitoring process that aims to identify people who have been potentially exposed and alert them. This is a critical component in building a comprehensive strategy as it adds an extra layer of defense against the spread of an infectious disease. According to recent research, mobile and wearable contact tracing apps show superior performance, leading to 52% fewer cases as compared to traditional methods.
With the start of COVID-19, tech giants Google and Apple joined forces to provide contact tracing APIs and enable interoperability between iOS and Android devices. By leveraging these APIs and real-time location systems (RTLS), public health agencies can enhance their solutions with contact tracing functionality to position and track individuals who have been in close physical proximity and have had prolonged contact with an infected person.
Source: BBC
Data aggregation
Infectious disease data is crucial in helping healthcare professionals support public health and forecast the peak and the overall trajectory of a disease outbreak. In an epidemiological context, there are three main sources of data:
- Medical records including EHRs/EMRs, lab results, insurance claim forms;
- User-generated data from social media and mobile phones, including self-reports of health, symptoms, etc.
- Crowdsourced data from volunteers and field investigations.
The challenge with these large datasets is that they are not standardized and can be difficult to interpret. Thus, it is imperative for an infection control solution to support various data formats while also ensuring high quality of data like checking for double data entry, outliers, and more.
Automated infection surveillance
Clinical infection surveillance underpins any successful infection control program, but conventional methods like manual chart review are extremely resource-intensive — infection control professionals spend up to 36% of their time on surveillance. In addition, traditional manual surveillance often underreports infection rates by as much as 20% for some infection types.
Automated clinical surveillance can significantly reduce the burden on healthcare specialists so that they can focus their efforts on prevention. A recent cohort study showed that leveraging artificial intelligence (AI) and neural networks for automated infection surveillance allowed to correctly detect 67 out of 73 patients with HAI. And as AI models are becoming more accurate and sophisticated, automated surveillance has the potential to save time and costs while improving HAI diagnostics.
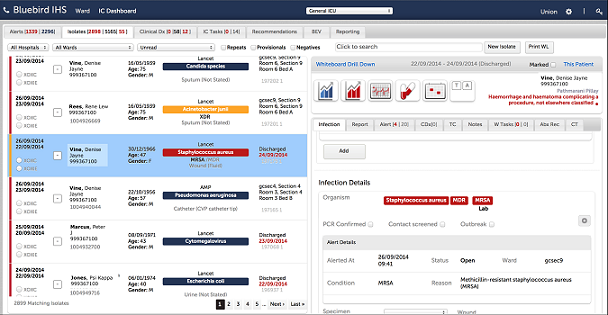
Real-time reporting
Once the data is collected and analyzed, it is important to make sure that it gets to the right people at the right time. Enhancing your infection control solution with powerful reports and interactive data visualization features helps healthcare practitioners glean valuable insights, identify trends, and make informed decisions faster.
In general, the more granular and customizable dashboards are, the easier it is for users to drill down to the specific area of interest like new infection cases, at-risk patients, admission dates, procedure codes, and more.
Source: Bluebird
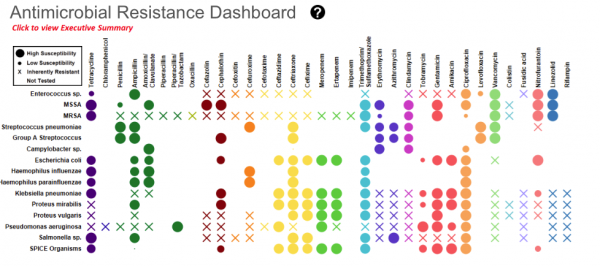
Antibiotic stewardship
Antibiotic resistance refers to the ability of bacteria to evolve over time and become resistant to the drugs designed to kill it. This is one of the most pressing health problems in the world, which is greatly exacerbated by antibiotics misuse and overuse, as well as poor infection control and prevention. The CDC estimates that at least 30% of antibiotics prescribed are unnecessary.
Antibiotic stewardship programs are designed to promote the responsible use of antibiotics while minimizing harm and drug costs. Integrating an antibiotic stewardship dashboard into an infection control solution arm clinicians with the necessary information to improve dosing, find a bug-drug mismatch, reduce unnecessary antibiotic therapy, and comply with Antimicrobial Use and Resistance (AUR) reporting rules.
Source: ReAct
The bottom line
Although COVID-19 has shaken the world to its core, it is not the first and definitely not the last global pandemic. Infectious diseases remain a clear and present danger to every country but especially to developing countries where the burden of epidemics on populations and economic growth is much higher than in high-income states — in no small part due to limited access to adequate healthcare.
There is a growing need for effective infection management measures to eliminate avoidable hospital-acquired infections and prepare for any future pandemic. And advancing technology can be our greatest defense. Robust infection control and prevention solutions can help health agencies and institutions stay on top of infection surveillance, early detection, warning, and management while freeing human resources to refocus on delivering safe and high-quality healthcare services.